ABOUT PARKINSON'S
Parkinson’s disease is a progressive, degenerative neurological condition that affects a person’s control of their body movements. In Australia, it affects 200,000 people with 38 people diagnosed every day.
It is important to note that not everyone will experience the same symptoms, and the order in which symptoms appear and the way symptoms progress also varies from person to person.
Additionally, non-motor symptoms such as sleep disturbance, constipation and loss of sense of smell can pre-date the motor symptoms, such as a tremor, slowness of movement or rigidity, by up to a decade.
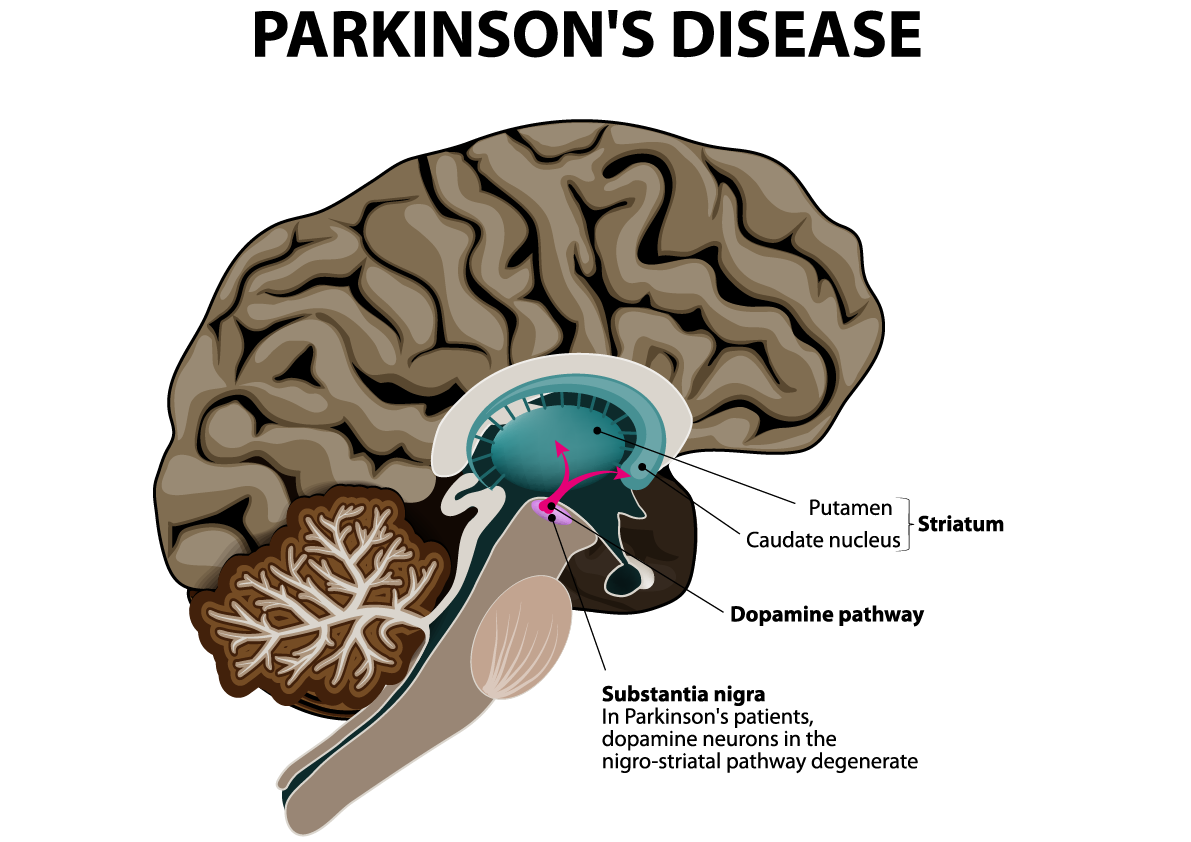
Parkinson’s results from the loss of cells in various parts of the brain, including a region called the substantia nigra. When dopamine production is depleted, the motor system nerves are unable to control movement and coordination. The dopamine producing cells are lost over a period of years and the motor type symptoms such as tremor, rigidity etc. will start to appear.
Australian Parkinson's Statistics
Parkinson’s disease is poorly understood. Many people associate the disease with an elderly relative or the odd celebrity on TV. The majority of the population understand it to be ‘just the shakes’. The reality is much different.
- Parkinson’s is the second most common neurological disease in Australia after dementia.
- The disease affects an estimated 10 million individuals worldwide – 200,000 in Australia.
- 38 Aussies are diagnosed with the disease every day.
- 20% of sufferers are under 50 years old and 10% are diagnosed before the age of 40.
- The number of people with Parkinson’s has increased by 17% in the last six years with costs to the community increasing by over 48%.
- For comparison purposes, the prevalence of Parkinson’s is greater than prostate, bowel, and many other forms of cancer and the total number of Parkinson’s sufferers is 4 times the number of people suffering from MS.
To review the full 2015 Deloitte Access Economics ‘Living with Parkinson’s disease’ report click here
* note key statistics have been updated to 2019 based on growth estimates included in the Living with Parkinson’s Disease: An updated economic analysis 2014.
Is Parkinson's Genetic?
In the past 10 years, researchers have identified a number of rare instances where Parkinson’s disease appears to be caused by a single genetic mutation. In these cases, the mutated gene is passed from generation to generation, resulting in a great number of Parkinson’s disease cases within an extended family. Mutations in the LRRK2 gene are the greatest genetic contributor to Parkinson’s disease discovered to date.
While many Parkinson’s patients report one or more family members with the disease, it is not always clear that one or several genes are the cause. Scientists currently believe that in the majority of cases, genetic and environmental factors interact to cause Parkinson’s disease. Research into this subject continues aggressively every day.
Other Risk Factors of Parkinson's
Because the causes of Parkinson’s disease are unknown, there is no scientifically validated preventive course to reduce the risk of its onset. The single biggest risk factor for Parkinson’s disease is advancing age. Men have a somewhat higher risk than women.
That being said, a number of studies have highlighted factors that are associated with either greater or lesser risk of Parkinson’s disease. For example, smoking and caffeine consumption have been associated with lower rates of Parkinson’s disease, while head injury and pesticide exposure have been associated with higher risk. While such studies do not definitively link these factors with Parkinson’s disease one way or another, they highlight areas where further research may guide us to risk-prevention or treatment strategies.
Our website contains more information on the specific symptoms of Parkinson’s which include:
- Symptoms of Parkinson’s
- Sharing your Diagnosis
- Dyskensia
- Dystonia
- Smell loss
- Diet & Exercise
- Dexterity
- Freezing of gait (FOG)
Shake It Up Australia has co-funded 71 Parkinson’s research projects across 22 Australian research institutes to the value of over $27.7 million.

Parkinson’s Treatments
Current medications or surgery options can help to manage Parkinson’s symptoms, but we don’t yet have any treatments that can cure, slow, stop or reverse the progression.
Living with Parkinson’s
Living with Parkinson’s does require re-adjustment as the disease slowly progresses. We share some valuable information to help you live a better life.
Sharing Your Diagnosis
A Parkinson’s diagnosis affects everyone. Learn more about some commonly raised questions such as, what effect will it have on my relationship, how do I tell my children etc.
Young Onset Parkinson’s Disease
It’s not just an old person’s disease. 20% of people diagnosed with Parkinson’s are under the age of 50. Learn more about Young Onset Parkinson’s.
Parkinson’s Caregiver Information
The information on this page provides guidance on what to expect from Parkinson’s caregiving and how to care for your own health.
OUR IMPACT