Dystonia
Dystonia is characterised by painful, prolonged muscle contractions that cause involuntary repetitive twisting and sustained muscle contractions. These result in abnormal movements and postures. The symptoms usually begin in one body region, such as the neck, face, vocal cords, an arm or a leg, and then may spread to other parts of the body. The severity varies from person to person. Many people who have dystonia can maintain a relatively normal lifestyle. Others may need full-time assistance.
What causes dystonia?
Dystonia likely results from dysfunction of a related brain region affected in parkinsonism, the basal ganglia, although the ultimate cause is not known. Further research is necessary to determine the various genetic, environmental or other underlying mechanisms that may play a role in causing dystonia.
Dystonia is a prominent symptom for people with Parkinson’s who have a mutation in the Parkin gene — one of a handful of Parkinson’s-implicated genes — though more research is needed to understand why this is the case.
Ask The MD - Dystonia
Some experts estimate that forty percent of people living with Parkinson’s disease experience dystonia as an early symptom or as a complication of treatment.
What is the relationship between Parkinson’s and dystonia?
Dystonia and Parkinson’s disease (or parkinsonism) are movement disorders that are closely related. Parkinsonism is a term used to describe any clinical presentation that manifests in the cardinal symptoms of Parkinson’s disease (tremor, rigidity and slowness of movement).
Main Types of Dystonia
There are two main categories of dystonia: primary and secondary (or non-primary). Primary dystonia is a condition in which dystonia is the only clinical feature. There is no evidence of cell death or a known cause. It is also known as idiopathic torsion dystonia. Primary dystonia is thought to have greater genetic contribution, even in the absence of a family history of dystonia. Among forms of primary dystonia, the most common (and the most debilitating) is generalised dystonia, which affects the legs or one leg and the trunk, plus other regions, most commonly the arms.
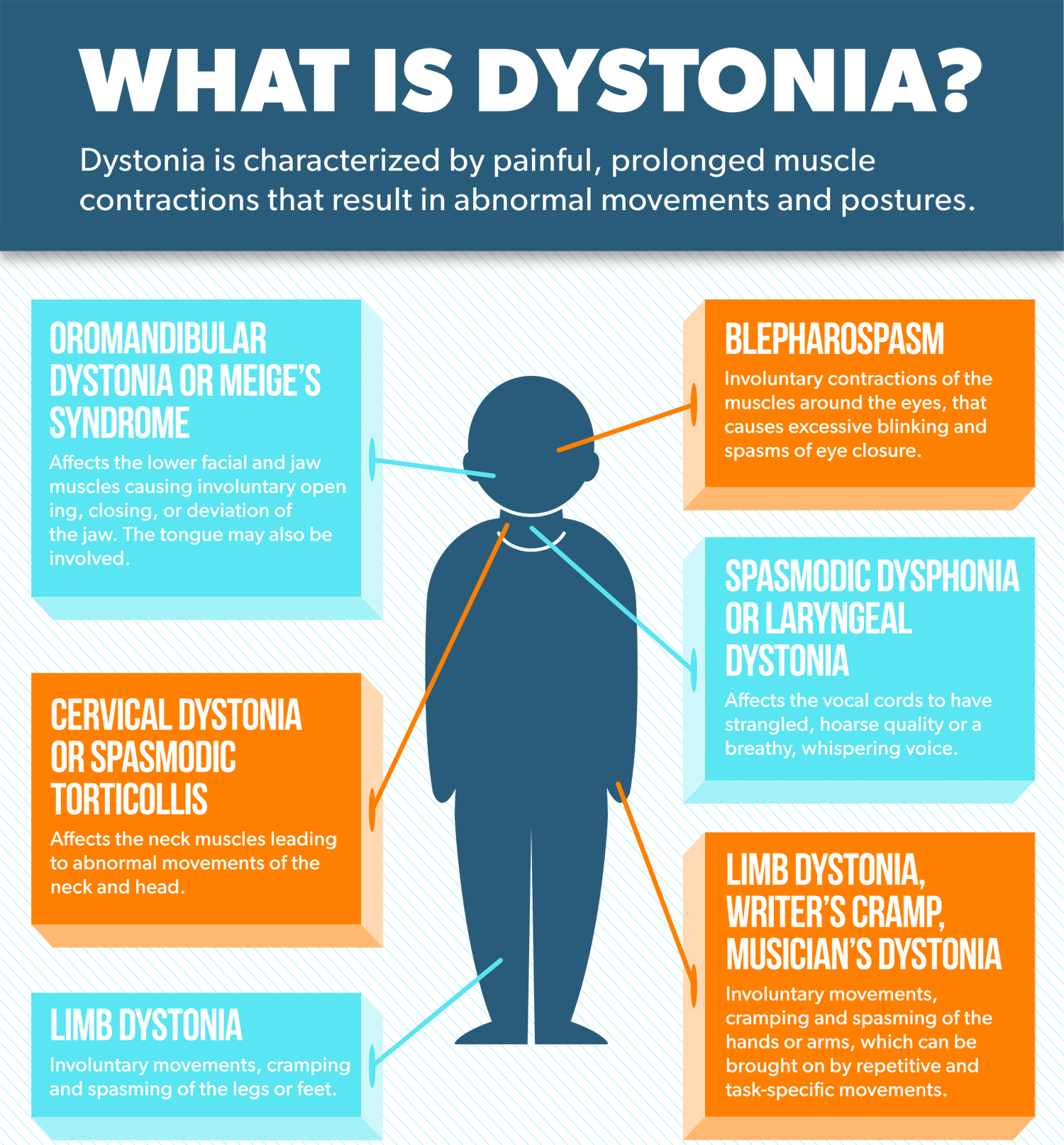
Outside the context of Parkinson’s disease, there are several other types of secondary dystonia, in which other symptoms are also present. In this category are:
- Myoclonus dystonia, characterised by dystonia and myoclonus (rapid, lightning-like muscle movements), with onset in childhood or adolescence.
- Dopa-responsive dystonia, a genetic disorder of childhood-onset and may have features of parkinsonism or exaggerated reflex responses.
- Rapid-onset dystonia parkinsonism, a rare inherited disorder characterised by sudden development of dystonia and parkinsonism.
- Paroxysmal dystonia, neurological conditions characterised by discrete and sudden episodes of involuntary movements.
Secondary dystonia may also be triggered by trauma to the head or a specific area of the body, drug use or exposure to rare toxins.
As in Parkinson’s disease, dystonia can be present in other neurological disorders including:
- Wilson’s disease, a rare genetic disorder in which copper accumulates in the organs.
- Huntington’s disease, a hereditary progressive neurodegenerative disorder.
- Spinocerebellar ataxias, a group of progressive degenerative inherited conditions.
- Methylmalonic aciduria, an inherited disorder of metabolism.
What treatments exist for dystonia?
Dystonia and Parkinson’s share common forms of treatment. Anticholinergic medications (such as trihexyphenidyl or benztropin) and levodopa may improve both conditions (though dystonia, like other Parkinson’s symptoms, can return or worsen as levodopa wears off and loses efficacy with long-term use). And deep brain stimulation (DBS) is a surgical treatment for both, although the stimulation target in the brain may be different.
Other medications such as muscle relaxants or antispastic agents may also treat dystonia. In addition, physicians may prescribe botulinum toxin injections. When a small amount of commercially prepared botulinum toxin is selectively injected in overactive muscles, it causes a change in the muscle firing, calming the abnormal movements for up to several months at a time.
Physical therapy may be helpful as a supplement to other therapies. Many patients report beneficial effects from complimentary therapies such as yoga, tai chi and meditation, although rigorous studies evaluating their efficacy are lacking.
What therapies are in development for dystonia?
For dystonia with Parkinson’s disease, researchers are working on better levodopa delivery. Optimizing the current standard of treatment to work more reliably and last longer would help treat dystonia related to Parkinson’s and avoid the medication wearing off and symptoms returning.
Podcast: Muscle Cramps with Parkinson’s
Does everyone with Parkinson’s get Dystonia
Not everyone with Parkinson’s gets dystonia, but it can happen at any point in the course of the disease. For people who do have dystonia, it can come on at different times throughout the day.
Dystonia is also more common in younger people with Parkinson’s, in people who are younger than 40 or 50, for example. It may even be the first symptom of the disease. Sometimes people with young or early-onset Parkinson’s first notice dystonia during exercise and then later develop other symptoms of Parkinson’s, like tremor or stiffness, that leads to the diagnosis.
Nikki was diagnosed with Parkinson’s at the age of 35 after noticing her toes curling and her foot aching.

